March 14, 2012
Medicare and Medicaid Fraud: a Targeted Problem in Need of a Targeted Solution
We recently had the opportunity to attend the Alliance for Health Reform briefing on healthcare fraud and prevention. It’s an important and timely topic for the home healthcare community. Our community recognizes that program integrity and payment reforms are needed to strengthen the Medicare and Medicaid programs and secure seniors’ access to quality healthcare services.


How Big is the Problem?


- 

- “Hundreds of billions of dollars in waste and fraud…” (President Obama speech to Joint Session of Congress, Sept. 9, 2009)
- “These schemes steal as much as $100 billion a year from Medicare and Medicaid…” (Newt Gingrich and AARP CEO Barry Rand, Orlando Sentinel, Sept. 29, 2010)
- “…Health care fraud and abuse (is) hundreds of billions per year…” (Harvard Professor Malcolm Sparrow, Senate Judiciary Committee, May 20, 2009)
- One-third of all health care spending is fraud, waste and avoidable inefficiencies (Institute of Medicine [2011] and Thomson Reuters [2009])
- Americans think 51 cents of every federal dollar spent is wasted (Gallup, September, 2011)












For additional information on the cost of health care fraud, please click here.


Fraud and Abuse is a Targeted Problem in Need of a Targeted Solution


The Partnership for Quality Home Healthcare is committed to working toward reforms that achieve significant savings and strengthen Medicare program integrity without harming seniors or cost-­efficient providers.


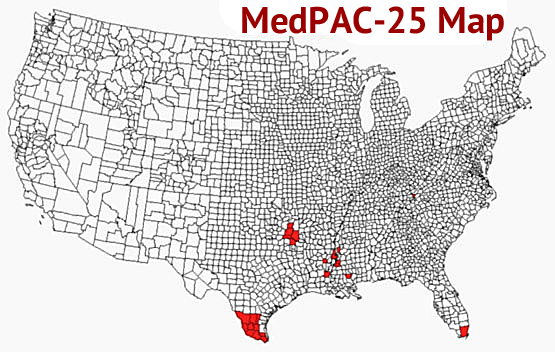
The Medicare Payment Advisory Commission (MedPAC) has identified 25 counties as having the highest prevalence of Medicare abuse in home healthcare:




The MedPAC data demonstrate that program integrity is a targeted problem. In response, the home healthcare community has developed bold reforms that offer a targeted solution.


Precedent: Medicare’s 10% Limit on Home Health Outlier Claims


In 2009, the home healthcare community proposed a Medicare reform limiting home healthcare outlier claims to 10% of a provider’s total reimbursement. This policy was adopted and has proven effective in achieving savings without harming seniors or cost-efficient providers.


Analysis of CMS’s recently released claims data for 2010 indicates that the Outlier Limit generated $853 million in savings in 2010 – equivalent to $11 billion in 10 year savings – without harming seniors or the vast majority of cost-effective providers who operate inside the national norms.


Our Proposal to Fight Healthcare Fraud


To fight fraud and strengthen program integrity, while protecting seniors who rely on home healthcare services, we propose payment reforms based on the Outlier Limit model:


- 

- Episode Limit: cap payment at a per-­provider average of 2.7 episodes per beneficiary (non-­rural) and 3.3 episodes per beneficiary (rural).




- 

- LUPA Limit: incorporate a minimum annual low utilization payment adjustment (LUPA) rate of 5% to all episodes payments.




To learn more about coordinated efforts to combat healthcare fraud by leading organizations representing America’s senior, disabled, minority and veteran populations, visit http://www.americansagainstfraud.org.